- Beta cells, which produce insulin in the pancreas, have been linked to the development of type 1 and type 2 diabetes
- A drug called harmine was found to multiply beta cell rates at about two per cent per day, 10 times more than our bodies do on their own
- But when given in combination with a drug responsible for bone formation, the rates increased to as much as eight per cent per day, 40 times more
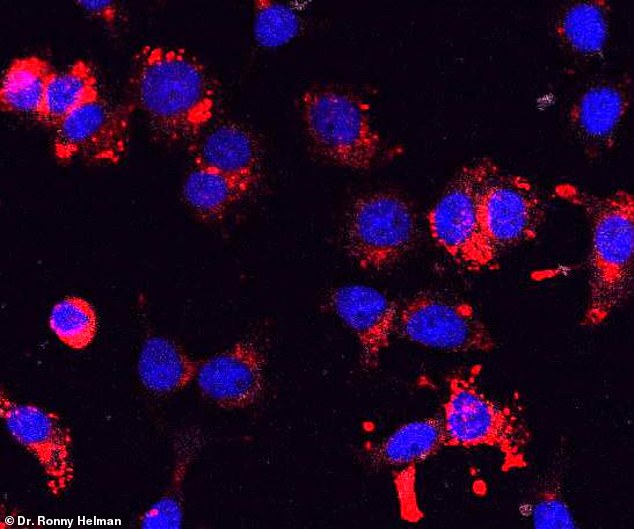
A newly-developed drug cocktail makes insulin-producing cells multiply – a discovery that could lead to a cure for diabetes, researchers claim.
People with diabetes have a shortage of beta-cells, which make insulin. Without enough insulin, they are unable to properly process glucose.
The team, from the Icahn School of Medicine at Mount Sinai Hospital in New York, had already discovered that a drug called harmine could supercharge the pancreas cells to make 10 times more insulin-making beta cells a day.
What’s more, when harmine was given in combination with a second drug – normally used to boost bone-growth – 40 times more beta cells formed a day.
The drug is experimental and in early stages of testing, but the researchers think that its powerful effect on insulin-producing cells could be a game-changer in the treatment of both type 1 and type 2 diabetes.
According to the Centers for Disease Control and Prevention, 30.3 million Americans – about 9.4 per cent of the population – suffers from diabetes.
Another estimated 84 million are living with prediabetes, a condition that can lead to type 2 diabetes within five years if left untreated.
Diabetes occurs when there are too few beta cells in the pancreas to produce insulin or when they produce very little insulin, the hormone needed to get glucose from the bloodstream into cells.
When left untreated, diabetes can result in serious health complications such as kidney damage, eye damage, heart disease, stroke and even vision loss.
The loss of beta-cells has been linked to causing type 1 diabetes, in which the immune system mistakenly identifies beta cells as invaders and destroys them.
More recently, scientists have discovered that having a deficient number of functioning beta cells can contribute to the development of type 2 diabetes.
 According to lead author Dr Andrew Stewart, director of the Mount Sinai Diabetes, Obesity, and Metabolism Institute, no available diabetes drug regenerates beta cells in patients with the condition.
According to lead author Dr Andrew Stewart, director of the Mount Sinai Diabetes, Obesity, and Metabolism Institute, no available diabetes drug regenerates beta cells in patients with the condition.
The current study is a continuation of past work done by Dr Stewart and his team.
In 2015, they published a study which found that a drug called harmine – found in the ayahuasca vine – helped produce new adult human beta cells at low rates.
A second study published in 2017 found genetic abnormalities in insulinomas, tumours of the pancreas that are derived from beta cells and secrete insulin.
The researchers discovered the tumours held a ‘genetic recipe’ of how to make beta cells regenerate.
In the current study, the team identified a second class of drugs that cause human beta cells to rapidly replicate when given in combination with harmine.
Without drug intervention, beta cells replicate an average rate of 0.2 per cent per day.
When harmine is administered, the rate is two per cent per day. But when harmine is given in combination with the new drug, this rate increases to between five and eight per cent per day.
‘We are very excited about this new observation because, for the first time, we are able to see rates of human cell beta cell replication that are sufficient to replenish beta cell mass in human beings,’ Dr Stewart said.
‘We have discovered a drug combination that makes beta cells regenerate at rates that are suitable for treatment. The next big hurdle is figuring out how to deliver them directly to the pancreas.’
Dr Stewart says one challenge, however, is that this drug combination has effects on other organs, although he didn’t specify what those effects were.
‘We now need to develop methods to deliver these drugs specifically to the beta cell in humans,’ he said.
‘We have the packages to deliver, but now we need a courier system to deliver them to the exact beta cell address.’
Source: Dailymail
 Based on +200
reviews
Based on +200
reviews


